This blog post is based on insights from Dr. Pal and Dr. Deepti Jamy’s YouTube video discussing PCOS, PCOD, fertility options, and women’s health. Their expert conversation provided the foundation for this educational content.
Have you ever found yourself frantically searching “why are my periods irregular” at 2 AM, only to spiral into a web of confusing diagnoses and scary stories? You’re not alone. Millions of women encounter the terms PCOS (Polycystic Ovary Syndrome) and PCOD (Polycystic Ovarian Disease) every year, often feeling overwhelmed by conflicting information.
Recently, Dr. Pal and Dr. Deepti Jamy sat down for an honest, eye-opening conversation about what these conditions actually mean—and the truth might surprise you. Contrary to popular belief, these aren’t life sentences or purely genetic curses. Instead, they’re often signals from your body that your lifestyle needs attention.
Let’s break down what these experts want every woman (and her partner) to understand about hormonal health, fertility, and taking back control.
PCOS vs PCOD: Clearing Up the Confusion
First things first: while doctors sometimes use these terms interchangeably in casual conversation, they’re not exactly the same thing. Understanding the difference is your first step toward effective PCOS treatment naturally.
What Do These Terms Really Mean?
PCOD is essentially a condition where your ovaries contain multiple immature or partially mature eggs that eventually turn into cysts. It’s often considered a milder, more manageable condition that responds well to lifestyle adjustments.
PCOS, on the other hand, is a full-blown hormonal imbalance and metabolic disorder. It involves excess androgen (male hormone) production, which disrupts your menstrual cycle and can cause a cascade of symptoms like acne, weight gain, and facial hair growth.
Think of it this way: all squares are rectangles, but not all rectangles are squares. Similarly, PCOS often includes PCOD-like symptoms, but PCOD doesn’t always develop into PCOS.
Why Dr. Google Can Be Dangerous
Here’s something both doctors emphasized strongly: Stop self-diagnosing through the internet.
“Every body is different, and what looks like PCOS on a symptom checklist might actually be thyroid issues, stress-induced hormonal changes, or something else entirely,” explains Dr. Deepti Jamy.
When you match PCOS symptoms online—like irregular periods, mood swings, or weight fluctuations—you might miss the bigger picture. Professional medical consultations include blood tests, ultrasounds, and a thorough understanding of your medical history. This matters because the wrong “treatment” can actually make things worse.
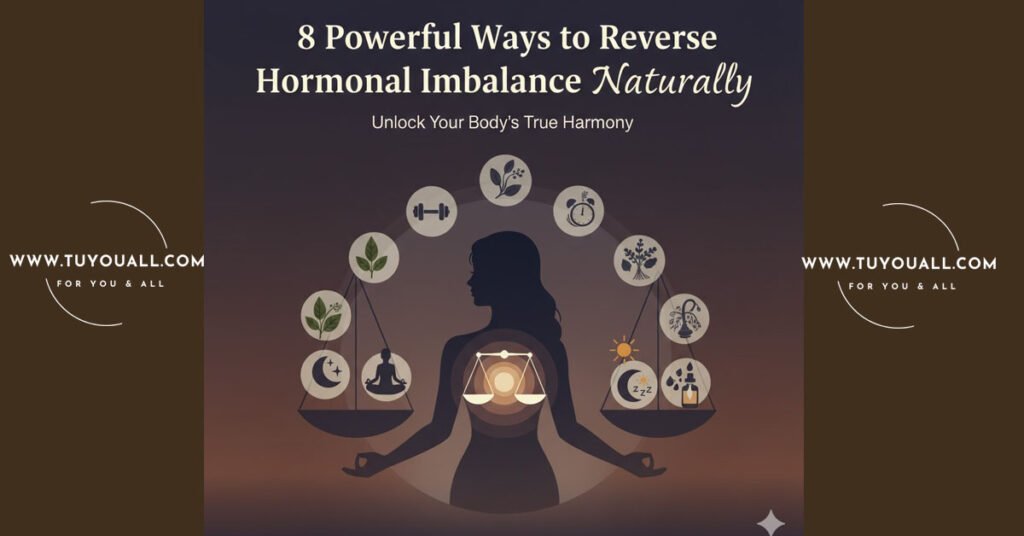
The Real Culprits Behind Hormonal Imbalance
If you’ve been blaming your genes or feeling like a victim of bad luck, here’s some empowering news: your lifestyle choices play a massive role in managing these conditions.
It’s Not Just “Bad Genes”
While genetics can predispose you to hormonal issues, they don’t write your destiny. Dr. Pal notes that the surge in PCOS cases over the last few decades correlates directly with modern lifestyle changes—not genetic mutations.
“We’re seeing younger and younger women with these issues, and it’s rarely because of family history alone. It’s about how we eat, sleep, and manage stress today,” he observes.
The Lifestyle Factors You Can Control
The good news? You have more control than you think. Here are the three pillars that can make or break your hormonal health:
- Diet Matters More Than Pills: Processed foods, excessive sugar, and irregular eating hours spike insulin levels, which worsens hormonal imbalance. Focus on whole grains, lean proteins, and plenty of vegetables.
- Stress is a Silent Hormone Disruptor: Chronic stress floods your body with cortisol, which directly interferes with reproductive hormones. That deadline anxiety? It’s affecting your cycle.
- Sleep is Non-Negotiable: Poor sleep patterns disrupt your circadian rhythm, which regulates everything from hunger hormones to fertility signals.
For example, consider a 28-year-old software engineer who works night shifts, survives on coffee and vending machine snacks, and checks work emails until midnight. Her irregular periods aren’t “just bad luck”—they’re her body’s SOS signal that these habits need changing.
| Lifestyle Factor | What to Avoid | What to Embrace |
| Eating Habits | Skipping meals, processed snacks, sugary drinks | Regular meal times, high-fiber foods, hydration |
| Stress Management | Constant multitasking, no downtime | Meditation, yoga, or even 10-minute walks |
| Sleep Hygiene | Screen time before bed, inconsistent bedtimes | 7-8 hours nightly, dark, cool bedroom |
Can You Get Pregnant with PCOS? Fertility Facts That Give Hope
One of the biggest fears women face after a PCOS diagnosis is infertility. But here’s what Dr. Deepti Jamy wants you to know: “Having PCOS doesn’t mean you can never conceive. It means you need to be more intentional about your health.”
Weight Loss as a Game-Changer
Even a 5-10% reduction in body weight can regulate your menstrual cycle and significantly improve ovulation. This isn’t about fitting into a certain dress size—it’s about reducing insulin resistance, which is often the root cause of PCOS-related infertility.
Start small: swap white rice for brown rice, take stairs instead of elevators, or try intermittent walking during work calls. These sustainable changes trump crash diets every time.
Tracking Your Cycle
Understanding your body’s unique rhythm is crucial for PCOS fertility tips that actually work. Unlike women with regular 28-day cycles, PCOS patients might ovulate less predictably.
Use apps, basal body temperature tracking, or ovulation predictor kits to identify your fertile windows. Knowledge is power here—when you know your body, you can time conception attempts more effectively.
Planning for the Future: Egg Freezing and Modern Options
Not ready to have babies yet? That’s completely valid. Whether you’re climbing the corporate ladder, pursuing higher education, or simply haven’t found the right partner, modern medicine offers options that previous generations didn’t have.
When Career Comes First
Egg freezing for career planning is becoming increasingly popular, and for good reason. Your egg quality and quantity decline significantly after age 35, but freezing them in your late 20s or early 30s preserves your fertility potential.
Dr. Pal explains: “Think of it as an insurance policy. You’re not committing to having children, but you’re keeping the option open for when you’re truly ready.”
The process involves hormone injections for about 10-12 days, a minor surgical procedure to retrieve the eggs, and then cryopreservation. While it’s an investment, many women find the peace of mind priceless.
Sperm Freezing for Men
Fertility preservation isn’t just a women’s issue. Men can freeze sperm samples, which is simpler and less expensive than egg freezing. This is particularly useful for men undergoing medical treatments that might affect fertility or those who want to delay fatherhood for personal reasons.
Why Your Partner Needs to Be Part of the Conversation
Here’s something that doesn’t get discussed enough: family planning and birth control are shared responsibilities.
Shared Responsibility in Birth Control
Too often, women bear the entire burden of contraception, from daily pills to IUD insertions. But as Dr. Deepti Jamy points out, “It takes two people to make a baby, so it should take two people to prevent one or plan for one.”
Men have options too—vasectomies (which are reversible in many cases), condoms, and participating in discussions about timing. When both partners understand the woman’s cycle and health conditions like PCOS, they can make better joint decisions.
Family Planning as a Team Sport
If you’re dealing with PCOS and trying to conceive, your partner’s support is crucial. This might mean:
- Adopting healthier eating habits together (rather than you eating salad while he eats pizza)
- Managing stress as a household
- Attending doctor’s appointments together
- Understanding that conception might take longer and requiring patience
“When men understand that PCOS is a metabolic issue, not just a ‘women’s problem,’ they become better allies in the journey,” says Dr. Pal.
Frequently Asked Questions
Q.1. What’s the main difference between PCOS and PCOD?
PCOD is primarily an ovarian condition involving cysts, while PCOS is a comprehensive hormonal and metabolic disorder affecting multiple body systems. PCOS typically requires more intensive management but both respond well to lifestyle changes.
Q.2. Can PCOS be completely cured?
There isn’t a permanent “cure,” but symptoms can be effectively managed and often reversed through consistent lifestyle modifications. Many women achieve regular cycles and healthy pregnancies after adopting better habits.
Q.3. Will I never get pregnant if I have PCOS?
Absolutely not. While PCOS can make conception more challenging, many women with the condition conceive naturally or with minimal medical assistance. Weight management and cycle tracking significantly improve your odds.
Q.4. Is egg freezing a painful procedure?
The process involves some discomfort from daily injections and mild cramping after retrieval, but it’s generally well-tolerated. Most women return to normal activities within a day or two after the procedure.
Q.5. How much sleep do I really need for hormonal balance?
Aim for 7-9 hours of quality sleep per night. Consistency matters more than perfection—going to bed and waking up at the same time daily helps regulate your body’s hormone production.
Conclusion
PCOS and PCOD might sound intimidating, but they’re ultimately your body’s way of asking for better care. By focusing on sustainable lifestyle changes—nutritious food, stress management, quality sleep, and professional medical guidance—you can reclaim control over your hormonal health and fertility.
Remember, you’re not broken, and you’re definitely not alone. Whether you’re managing symptoms today or planning for motherhood tomorrow, small, consistent steps lead to big transformations.
Credit Section:
This blog post is based on insights from Dr. Pal and Dr. Deepti Jamy’s YouTube video discussing PCOS, PCOD, fertility options, and women’s health. Their expert conversation provided the foundation for this educational content.